Shift Staff Knowledge, Attitudes & Beliefs
One key to success is normalizing HIV testing, changing the perception that it’s a specialty thing. It needs to be part of routine health care maintenance.
– Chief of Psychiatry and former Medical Director, Brookwood site
Supplement Staff Knowledge
Don’t assume that staff know all the facts about HIV. Front desk staff and MA’s, in particular, likely need to learn more about HIV. Focus on misconceptions and dispelling myths. Teach everyone:
| |
Why it’s important to get tested |
 |
That you can’t tell if someone has HIV by looking at them. |
 |
To be comfortable speaking with patients about HIV and answering role-appropriate questions, and knowing where to access information that might be beyond their understanding or scope. |
 |
How HIV is and isn’t transmitted (fluids, high-risk behaviors) |
 |
That HIV is not a death sentence thanks to anti-retroviral medications, and under proper care, patients with HIV can live long active lives |
PrEP and nPEP should also be covered. Staff should know what they are and when and how to refer for them. Front desk staff needs to know the services offered, how to talk about them, and how to listen for cues that would indicate need for an urgent HIV nPEP appointment. Providers need information on PrEP. Patients often reveal something different to each staff member, and by the time they get to the provider they are more open, more likely to share something that indicates a need for PrEP.
Shift Staff Attitudes and Beliefs
Have staff approach HIV testing from a harm reduction model and encourage non-judgmental, supportive care. Our motto was “Know your health, know your status.” We would test everyone regardless of age (15 and older), sex, gender, sexual preference, income, etc. Make sure everyone understands that:
- HIV doesn’t only affect sex workers, intravenous drug users, and homosexual men. It does not discriminate.
- HIV can be eradicated from our community through early diagnosis and proper care.
- Everyone with HIV deserves high quality health care free from stigma.
Use Different Activities to Engage Everyone
A typical training might provide 45 minutes of project overview, dialog, an HIV Knowledge Attitudes Beliefs (KAB) exercise and group discussion, plus a product representative reviewing testing procedures. It’s not a lot of time so it must be used wisely. Here are a few activities we found helpful:
- Culture change happens through the changing stories we tell ourselves, so collect and share stories about patients who tested positive.
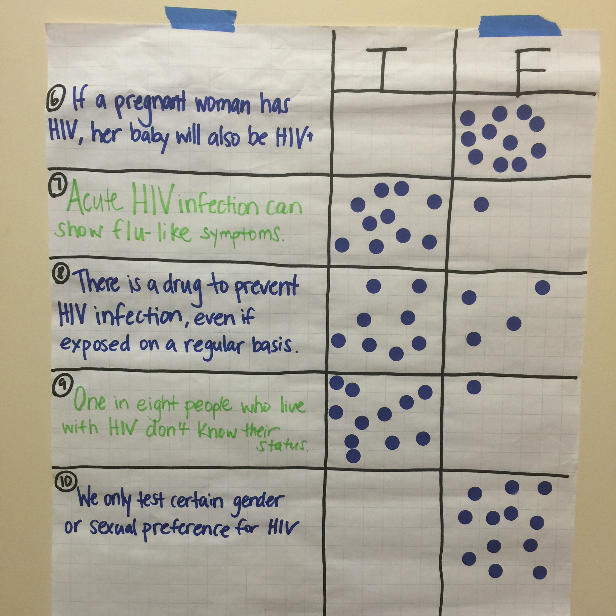
Figure 16. Group KAB activity - Get people up and moving. For example, give people stickers to place on a list of true and false HIV statements and ask them to place their sticker to indicate the right answer. This allows for some anonymity of responses, helping to provide honest answers rather than “group think” responses.
- Generating discussion among staff increases engagement. Try exercises that help to generate questions. For example, having staff answer potentially controversial questions anonymously, like the exercise shown in Figure 16, can lead to interesting discussions. A slightly faster alternative is to ask everyone to anonymously complete a paper form, then mix up the pages and grade an anonymous person’s responses. Be sure to collect the forms so later you can tally responses and take the pulse on what topics were widely known and what topics need more attention.
You can also use a tool like SurveyMonkey to anonymously survey staff more widely to determine their current knowledge, attitudes and beliefs. Distributing paper surveys is an option although SurveyMonkey can save time because it tallies the results automatically.
Facilitate group discussion by breaking people into small groups and providing them a list of questions to talk about. For example, during MA training people could discuss:
-
- What might stand in the way of opt-out HIV testing?
- What is one way you can break through this barrier?
- What is one success you’ve had when offering HIV opt-out testing?
- Practice dialog. Reinforce newly learned facts by having staff practice explaining the information to one another as they would to patients.
- Build on expertise gained from previous experience. For example, MAs working in a Title X (federal family planning program) setting may already be more comfortable discussing sensitive topics with patients. Build from their existing skills to provide more advanced education.
A Quick Clinic Story: Harm Reduction in Action
Here’s a story our Senior Nurse Manager told us about one typical patient interaction:
“Recently I was pulled into the clinic for patient care when we were understaffed. I was caring for a young woman in her 20’s with multiple sex partners in the last year, condomless sex, and re-infected to chlamydia and gonorrhea.
I provided education on behaviors that put her at risk in a non-judgmental (harm reduction) way, and did a follow-up call the next day to inform on PrEP. I told her, ‘Science has come a long way and this may be something you want to consider… no judgment, have fun, and my only hope for you is that you know how to stay safe and protect yourself as well.’ The information on PrEP kind of landed that her behaviors were putting her at higher risk, woke her up a bit maybe.
Being prepared made the visit easier: I knew the patient was re-infected, so I printed education materials, downloaded the template into the chart prior to the visit, and brought meds. All of this allows focus on the priority objectives to be handled efficiently so the conversation can go into other points of education and focus. It’s easy to get off track with patients otherwise. It’s always a difficult conversation to have, even with all of the education.
Roleplays and increasing practice is helpful to increase comfort levels over time in all staff. It’s also helpful having support to debrief the appointment after, to think about, “Did I sound judgmental? Did I cover all of my bases?”
Resources
- HIV Training Video – HIV Overview: Introductory video on Understanding HIV and AIDS. Describes HIV and AIDS and why testing matters (.mov)
- HIV Training Video – FAQs: Frequently Asked Questions about HIV and AIDS (.mov)
- HIV Training Slides – True-False Questions: Test staff knowledge with these training slides with a series of statements that are either true or false (.pdf or .pptx)
- News Report – Normalizing HIV: New report on efforts to normalize HIV testing (link)
- HIV does not kill. STIGMA does!: Video with an HIV positive person discussing stigma of HIV virus, how it has affected her life, and why it shouldn’t exist (link)
- Basics of ART nPEP & PrEP: Fact sheet on PrEP, nPEP and HIV treatments (.pdf)
- Online Staff Survey Contents: Sample staff survey about HIV testing, including feedback on trainings, changes in knowledge and beliefs, overall success of screening efforts and barriers to screening, patient response, and usefulness of promotional materials, (.pdf or .doc)
![$logo['alt']](https://srhealth.org/wp-content/uploads/2017/03/srch-logo-1.png)